What Is Endoscopic Healing? Procedure, Purpose and What to Expect

What is an endoscopy?
Endoscopy is the umbrella term for a group of medical procedures that use an endoscope, a long, thin tube with a small camera, that is inserted into the body through a natural opening like the mouth or the anus.1 It is considered as the gold standard for measuring disease activity in IBD, playing an important role in diagnosis, management, and treatment of
You may be referred for an endoscopy if you have any IBD symptoms.
There are different types of endoscopy procedures, such as:
A procedure that examines the entire large bowel to diagnose or screen for conditions like colorectal cancer and inflammatory bowel disease1
A quicker, lower-bowel-focused exam of the rectum and sigmoid colon, often used for targeted investigations or screening3
An upper GI test that uses a flexible camera to assess the oesophagus, stomach, and duodenum for ulcers, reflux, or coeliac disease4
Why are endoscopies so important?
Endoscopy plays a key role in diagnosis, monitoring of disease activity, assessment of treatment response, and ultimately guiding treatment decisions.1 Endoscopies help in showing the inflammation that might not be reflected by symptoms, as inflammation doesn’t always cause obvious symptoms. In some cases, even when symptoms improve, inflammation may still be active inside the gut. Endoscopies allow healthcare professionals to look directly at the bowel lining to assess the severity of diseases such as Crohn’s disease (CD) or ulcerative colitis (UC), to see if healing is occurring.5
Endoscopies also play a role in IBD treatment.15 Findings made following an endoscopy can also help to tailor treatment plans. Depending on whether or not healing is seen within the gut lining, your care team might make adjustments to your treatment, before a flare-up has the chance to occur.6

How does an endoscopy compare against other types of tests?
Endoscopy provides the clearest, most accurate view of inflammation in the gut, making it an essential tool for diagnosing and monitoring CD and UC. Unlike stool or blood tests (which can show signs of inflammation but not its exact location or severity) and scans like MRI or CT (which miss surface-level changes), endoscopy offers direct visual confirmation of disease activity and healing.5
That said, it’s rarely used alone. Most often, your care team will combine endoscopy with other tests, such as biopsies, blood work, and stool analysis. Less invasive tools like intestinal ultrasound are also increasingly being used to assess inflammation without the need for sedation or bowel prep.5

What is endoscopic healing?
Therapeutic goals in IBD have evolved beyond just looking at controlling symptoms, to include endoscopic healing, as a measure of treatment efficacy and healing at the mucosal lining level.6
Endoscopic healing refers to the absence of ulcers or erosions in the gut lining during an endoscopy. It's a sign that the inner lining of your intestines is healing, even if symptoms have improved.6
Some treatments are now designed to aim for endoscopic healing, not just symptom relief.
Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) is a program designed to examine potential treatment targets for IBD to be used for a ‘treat-to-target’ approach.7
STRIDE-II now includes endoscopic healing as a measure for treatment efficacy, shifting focus from durable symptomatic remission to true disorder modification.7
Why is endoscopic healing important?
Patients with endoscopic healing have better long-term clinical and patient-reported outcomes.6 Endoscopic healing is associated with:
Significantly better long term results without needing steroids.68
Fewer symptoms and better quality of life.68
Lower chance of relapses and better health over time.69
If you’re living with CD or UC, a healthcare professional may talk to you about setting goals for your treatment. These goals can support with guiding your care and tracking progress over time, these can be based on STRIDE-II and fall into three goal stages:7
Programma
Condition | Short-Term Goal | Medium-Term Goal | Long-Term Goal: Endoscopic Healing |
|---|---|---|---|
Crohn’s Disease | 50% reduction in abdominal pain and stool frequency | No abdominal pain and no more than 3 bathroom visits a day | No ulcers in your intestines |
Ulcerative Colitis | 50% reduction in rectal bleeding and stool frequency | No bleeding and fewer than 3 bathroom visits a day | Gut lining is smooth and healthy |
How do I know if endoscopic healing is taking place?

- Usually evaluated through a colonoscopy or sigmoidoscopy.
- Healthcare professionals look for ulcers, bleeding, redness, or other signs of inflammation.
- Your healthcare professional may use scoring systems to track healing over time.
- You might feel fine, but your healthcare professional may still want to check for deeper healing.
- Talk with your healthcare professional about whether endoscopic healing is a goal of your current treatment plan.
How can I prepare for an endoscopy?
- Follow your healthcare professional’s instructions exactly. You will receive specific guidance on when to stop eating and how to take bowel preparation. Make sure you stick to it, as an incomplete preparation could mean that you have to repeat the procedure.
- Plan for a clear liquid diet. Usually, the day before your endoscopy, you’ll need to switch to clear liquids only (e.g., water, apple juice or clear sports drinks)
- Stay close to a bathroom during prep. Once you start the laxative prep, it will work quickly. Wear comfy clothes, keep wet wipes nearby, and stay near a toilet.
- Talk to a healthcare professional about your medications. Some medications may need to be stopped or adjusted before the procedure. Always check ahead of time.
- Write down your questions. Write down anything you want to ask your healthcare professional about what they’re looking for, what you can expect to happen during the procedure, what the results might mean, or what comes next.
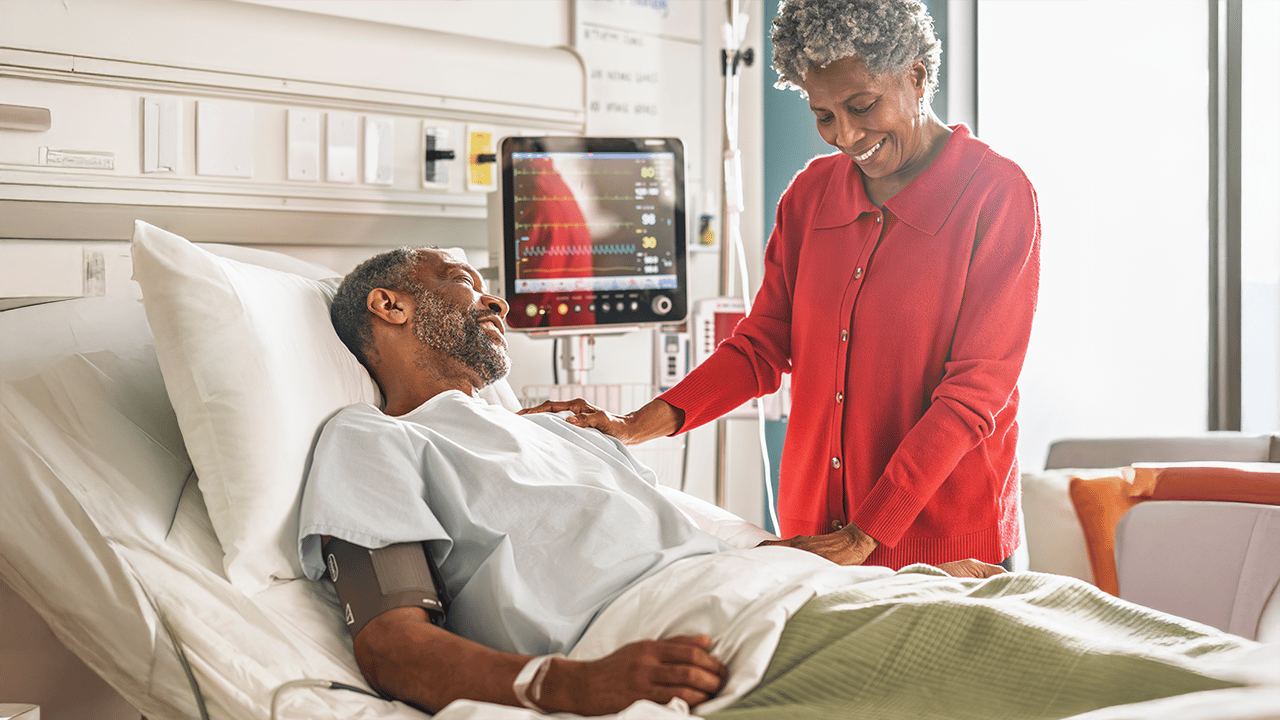
- Arrange for someone to take you home. You’ll likely be sedated for the procedure, which means you won’t be allowed to drive, and it might not be safe for you to traverse public transport on your own.
- Expect to feel groggy afterwards. Most people will feel sleepy for a few hours post-endoscopy, and you may feel mild cramping or bloating. Plan for a relaxed rest of the day.
Related content

Daily Life, Diet and Support

Understanding Your Options for Relief and Long-Term Management